Gynecology
Women through every rhythm of life, from managing PCOS and supporting fertility to caring during pregnancy and guiding hormonal wellbeing in menopause. With a science rooted in empathy, we aim to make every stage a step towards balance and comfort.
Products
PCOS (Polycystic Ovary Syndrome)
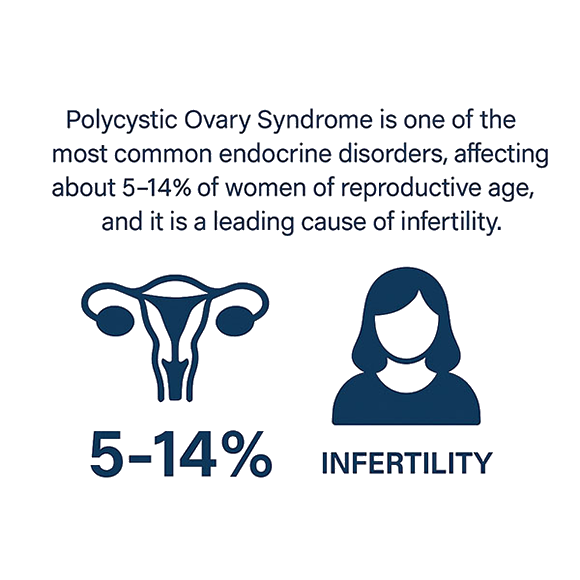
PCOS (Polycystic Ovary Syndrome)
PCOS is a chronic condition that affects women of reproductive age.
It usually starts during adolescence, but symptoms may fluctuate over time.
Interest in PCOS is constantly increasing due to growing evidence that it goes far beyond being only a reproductive disorder.
PCOS in women of reproductive age up to
1. A brief insight into the etiology, genetics, and immunology of polycystic ovarian syndrome (PCOS). Journal of Assisted Reproduction and Genetics 39, 2439–2473 (2022).
https://doi.org/10.1007/s10815-022-02625-7
This review highlights PCOS as a multifactorial disorder driven by the interaction between genetic predisposition, insulin resistance, hyperandrogenism, and chronic low-grade inflammation, leading to impaired follicular development, metabolic dysfunction, and infertility.
Infertility
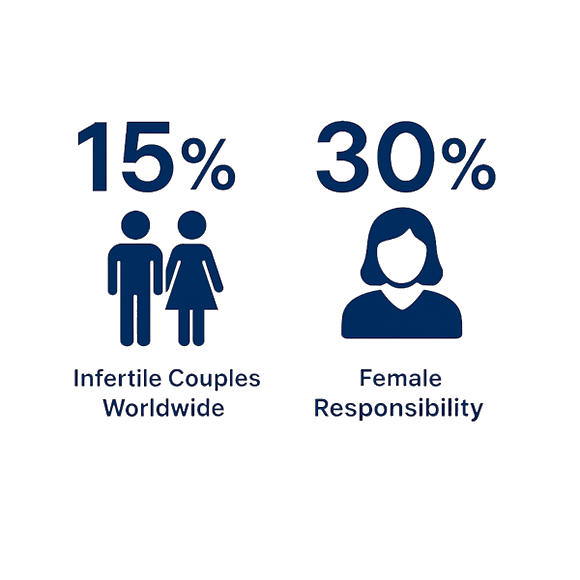
Infertility
Infertility is defined as “a disease of the reproductive system characterized by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse.”
15% of couples worldwide are infertile
Female infertility contributes to 30% of cases
15% — Infertile couples worldwide
30% — Female responsibility
Infertility affects around 70–80% of women with polycystic ovary syndrome (PCOS), primarily due to chronic anovulation and hormonal imbalances that disrupt normal ovulatory cycles and compromise oocyte quality.
The most common underlying causes include oligo- or anovulation, tubal obstruction, and implantation failure. Nevertheless, a significant proportion of women experiencing fertility issues still receive no definitive explanation for the origin of their reproductive dysfunction.
1. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Human Reproduction 22, 1506–1512 (2007).
https://doi.org/10.1093/humrep/dem046.
This review defines infertility as a disease of the reproductive system characterized by the failure to achieve a clinical pregnancy after 12 months of regular unprotected intercourse. It highlights female infertility as a major contributor to reproductive failure, primarily driven by ovulatory disorders (including PCOS), tubal disease, and implantation failure, while also emphasizing that a substantial proportion of cases remain unexplained despite thorough clinical evaluation.
Vaginal infections
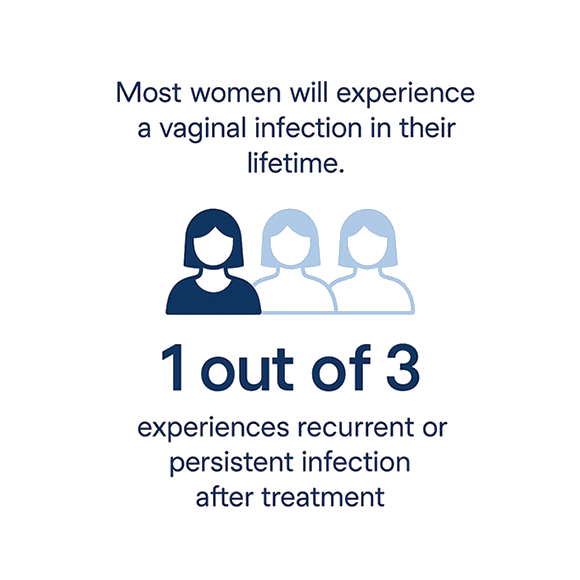
Vaginal Infections
Vaginal infections represent one of the most common gynecological conditions in women of reproductive age, often resulting from an imbalance in the vaginal microbiota and associated with significant discomfort and reproductive complications
Around 30% of women of reproductive age suffer from bacterial vaginosis or candidiasis. In fact, up to 75% of sexually active women experience at least one episode of symptomatic vaginal candidiasis during their lifetime, and approximately 35% face a relapse during pregnancy.
These infections are among the leading causes of reproductive complications and treatment failure.
1.
A new approach for the treatment of bacterial vaginosis: use of polyhexamethylene biguanide. A prospective, randomized study. A new approach for the treatment of bacterial vaginosis: use of polyhexamethylene biguanide. A prospective, randomized study – PubMed
The article reports a prospective, randomized clinical study evaluating intravaginal polyhexamethylene biguanide (PHMB) as a new treatment approach for bacterial vaginosis, comparing its efficacy with standard therapy.
The results show that PHMB achieved clinical and microbiological cure rates comparable to conventional antibiotic treatment, with good tolerability, suggesting it may represent an effective non-antibiotic alternative for BV management.
Menopause
Menopause
Menopausal women currently represent about 26% of the global female population, a figure projected to reach 1.65 billion by 2050.
This transition is accompanied by profound metabolic and physiological changes that significantly affect women’s health and quality of life.
Up to 60% of menopausal women are at risk of developing metabolic syndrome, while around 80% experience vasomotor symptoms such as hot flushes and night sweats. Menopause is also associated with an increased risk of cardiovascular disease, with studies indicating over a 48% rise in disease severity linked to the timing and intensity of menopausal symptoms. Furthermore, bone health is notably impacted: approximately 37.5% of postmenopausal women face an increased risk of developing osteoporosis. These data highlight the importance of early prevention, lifestyle interventions, and targeted therapeutic strategies to support women through the menopausal transition.
1. Effects of myo-inositol supplementation in postmenopausal women with metabolic syndrome: a prospective, randomized, placebo-controlled study. Menopause 18, 102–104 (2011). https://doi.org/10.1097/gme.0b013e3181e8e1b1
This randomized, placebo-controlled study shows that myo-inositol supplementation significantly improves key metabolic parameters in postmenopausal women with metabolic syndrome, including insulin sensitivity and lipid profile, supporting its potential role as a safe and effective nutritional approach for managing metabolic alterations associated with menopause.
Osteopenia / osteoporosis
Osteopenia & Osteoporosis
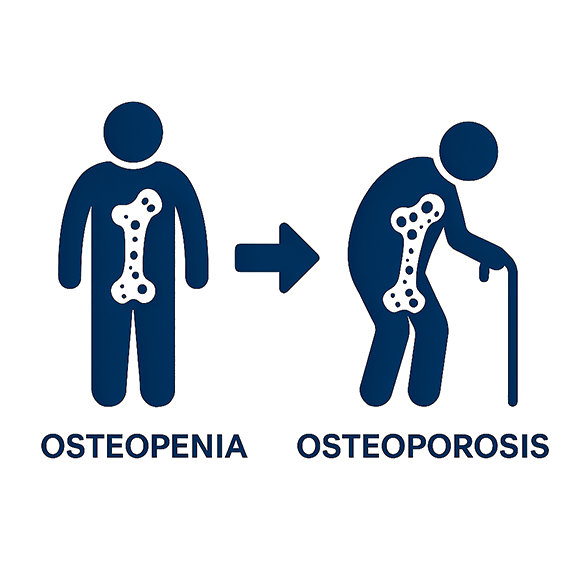
Osteopenia and osteoporosis are closely linked to gynecologic health, particularly during menopause, when declining estrogen levels accelerate bone loss.
Estrogen plays a key role in maintaining bone remodeling balance by inhibiting bone resorption; as its production drops in the menopausal transition, bone turnover becomes unbalanced, leading first to reduced bone density (osteopenia) and, in more advanced stages, to fragile, fracture-prone bones characteristic of osteoporosis.
Understanding this hormonal connection is essential for early identification of at-risk women and for implementing preventive strategies such as lifestyle modification, adequate calcium and vitamin D intake, and when appropriate, hormonal or non-hormonal therapeutic interventions.
1. Weitzmann MN, Pacifici R. Estrogen deficiency and bone loss: an inflammatory tale. J Clin Invest. 2006 May;116(5):1186-94. doi: 10.1172/JCI28550. PMID: 16670759; PMCID: PMC1451218. (Estrogen deficiency and bone loss: an inflammatory tale – PMC)
This review shows that estrogen deficiency accelerates bone loss by increasing osteoclast activity, with trabecular bone loss rates of up to 2–5% per year and a two- to threefold rise in pro-inflammatory cytokines.
2. Yang Lei, Li Misi, Chen Xiaoyun, An Yangxin, Hu Xueqin, Li Weijuan, New advances in the study of postmenopausal osteoporosis and arteriosclerosis: Exploration of metabolite changes and their mechanisms, Archives of Gerontology and Geriatrics Plus, Volume 2, Issue 4, 2025, 100222, ISSN 2950-3078, https://doi.org/10.1016/j.aggp.2025.100222. (New advances in the study of postmenopausal osteoporosis and arteriosclerosis: Exploration of metabolite changes and their mechanisms – ScienceDirect)
This review shows that postmenopausal women experience annual bone loss of about 1–3% and identifies metabolite alterations linking osteoporosis with increased cardiovascular risk.
Vaginal affections
Vaginal Affections
Vaginal affections are highly prevalent and can arise from multiple causes, including hormonal changes, infections, radiotherapy, or chronic inflammation. Up to 60% of women experience symptoms such as dryness, irritation, or discomfort, while approximately 20% of the overall female population may develop persistent vaginal disorders that compromise quality of life.
These conditions are often accompanied by morphological alterations—such as thinning of the vaginal mucosa, loss of elasticity, and reduced lubrication—that can affect both intimate and daily well-being. Following radiotherapy, the local tissue damage may further aggravate dryness and discomfort, leading to significant physical and emotional distress.
Effective physical and local treatments can play a crucial role in restoring tissue integrity, relieving symptoms, and improving overall comfort and confidence.
1.
Effectiveness and safety of vaginal suppositories for the treatment of vaginal atrophy in postmenopausal women: an open, non-controlled clinical trial. European Review for Medical and Pharmacological Sciences 12, 411–416 (2008).
https://pubmed.ncbi.nlm.nih.gov/19146203/
This open-label clinical study shows that local vaginal suppositories are effective and well tolerated in postmenopausal women with vaginal atrophy, leading to significant improvement in vaginal dryness, discomfort, and overall quality of life, and supporting the role of local therapy as a targeted and safe approach for managing menopausal vaginal symptoms.
HPV

HPV
Human Papillomavirus (HPV) infection is one of the most common sexually transmitted infections worldwide, with an estimated over 80% of sexually active women acquiring at least one HPV infection during their lifetime. In gynecology, persistent infection with high-risk HPV types is the primary cause of cervical cancer and is also associated with precancerous cervical lesions, as well as vulvar and vaginal neoplasia.
Beyond oncogenic risk, HPV can manifest clinically through benign epithelial changes and external genital lesions, such as condylomas (genital warts), which may impact quality of life and psychological well-being. Understanding the widespread prevalence and diverse clinical presentations of HPV is essential for early identification of at-risk women and for implementing preventive strategies, including vaccination, regular screening programs, and timely management of both precancerous and dermatological manifestations.
1. Human papillomavirus and cervical cancer. The Lancet 382, 889–899 (2013). https://doi.org/10.1016/S0140-6736(13)60022-7.
This review describes the clinical spectrum of HPV infection in women, highlighting that most infections are asymptomatic, while symptomatic disease may include genital warts caused by low-risk HPV types and cervical or lower genital tract lesions associated with high-risk HPV. Persistent infection can lead to precancerous changes and cancer, which are often clinically silent and detectable only through screening, underscoring the importance of early diagnosis and monitoring.
