Andrology
Alongside men in every phase of their reproductive health, from supporting fertility and hormonal balance to promoting vitality and wellbeing. Our commitment lies in helping men rediscover strength and confidence through science that truly cares.
Infertility
Infertility
Infertility affects approximately 15% of couples worldwide, and in 20–70% of cases, a male factor is involved—either as the sole cause, in idiopathic infertility, when both partners are affected, or in cases of recurrent miscarriage.
This growing burden has led to what is often described as the “Male Fertility Crisis.” Over the past decades, research has shown a more than 50% decline in sperm counts since the mid-1970s, accompanied by reductions in other semen quality parameters. Today, it is estimated that over 30 million men suffer from infertility globally, with numbers expected to rise if current trends continue.
Semen abnormalities such as oligospermia (sperm count < 15 million/ml), asthenospermia (total motility < 40% or progressive motility < 32%), and teratospermia (normal morphology < 4%) are major contributors to reduced male fertility.
The combination of these three—known as OAT syndrome (oligo-astheno-teratospermia)—is among the most common causes of male infertility. In 30–45% of cases, the underlying mechanism remains idiopathic, with no identifiable cause. Importantly, poor sperm quality can also compromise the success rates of assisted reproductive technologies (ART), making early assessment and intervention crucial for reproductive outcomes.
1. Male infertility. The Lancet 397, 319–333 (2021). https://doi.org/10.1016/S0140-6736(20)32667-2
This comprehensive review describes male infertility as a complex and multifactorial condition resulting from genetic, hormonal, infectious, environmental, and lifestyle-related factors. The authors highlight that impaired spermatogenesis, sperm DNA damage, oxidative stress, and genital tract infections are among the most common underlying mechanisms, while a substantial proportion of cases remain idiopathic despite advanced diagnostic evaluation.
HPV
HPV
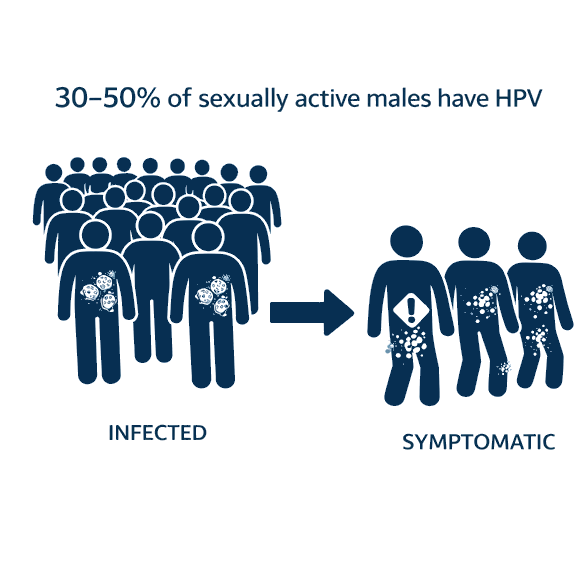
Human Papillomavirus (HPV) infection is equally prevalent in men, with global studies indicating that approximately 30–50% of sexually active males are infected at any given time, often without symptoms. In andrology, HPV affects the genital epithelium and can lead to cutaneous and mucosal manifestations, including genital warts, penile lesions, and other dermatological signs such as verrucous or vesicular-appearing growths.
In addition to visible lesions, HPV infection in men has been associated with alterations in sperm parameters, increased sperm DNA fragmentation, and potential implications for fertility. Since men frequently act as asymptomatic carriers, recognizing both the clinical and dermatological effects of HPV is crucial for comprehensive reproductive health care and for promoting prevention through vaccination, sexual health education, and appropriate clinical evaluation.
1. Epidemiology of human papillomavirus infection in men, cancers other than cervical and benign conditions. The Lancet Infectious Diseases 11, 877–890 (2011). Epidemiology of human papillomavirus infection in men, cancers other than cervical and benign conditions – PubMed
This review describes HPV infection in men as highly prevalent and frequently asymptomatic. When clinically apparent, HPV may cause external genital warts, penile and anal lesions, and, less commonly, symptoms such as pruritus, discomfort, or bleeding. Persistent high-risk HPV infection is associated with penile, anal, and oropharyngeal cancers, which often develop without early symptoms, highlighting the role of men as both affected individuals and silent carriers of HPV.
