Endocrinology
The complex connection between hormones and metabolism, for both women and men. From managing insulin resistance and osteopenia to restoring metabolic balance, our approach combines innovation and evidence-based care to sustain long-term health and energy.
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is a complex condition often associated with hormonal imbalance that affects both reproductive and metabolic functions. This imbalance can alter the normal regulation of ovarian activity, leading to irregular ovulation and changes in hormone levels that influence the menstrual cycle, skin, and overall metabolism. The interaction between reproductive and metabolic hormones plays a key role in many of the symptoms observed in PCOS, including cycle irregularities, acne, excess hair growth, and difficulties in conceiving. Over time, these hormonal disturbances may also contribute to weight fluctuations and metabolic complications, highlighting the importance of early recognition and appropriate management.
1. Journal/Review Article (2025) An endocrinological perspective on polycystic ovarian syndrome – ScienceDirect
This recent review emphasizes PCOS as a multifactorial endocrine disorder involving dysfunctions across multiple hormone systems, particularly the hypothalamic–pituitary–gonadal (HPG) axis, with altered gonadotropin-releasing hormone (GnRH) pulsatility leading to an elevated luteinizing hormone (LH) to follicle-stimulating hormone (FSH) ratio, which drives hyperandrogenism, impaired follicular development, and anovulation. It also discusses contributions from the hypothalamic–pituitary–adrenal (HPA) and hypothalamic–pituitary–thyroid (HPT) axes, showing how broader endocrine interactions and insulin resistance aggravate hormonal imbalance and metabolic complications in PCOS.
Thyroid subclinical disorders
Thyroid Subclinical Disorders
The thyroid is a small, butterfly-shaped gland located in the neck that regulates metabolism, energy, and growth through the production of thyroid hormones—triiodothyronine (T3) and thyroxine (T4).
Its activity is controlled by the hypothalamic-pituitary-thyroid (HPT) axis. When the gland fails to produce sufficient hormones, hypothyroidism occurs; when it produces too much, the result is hyperthyroidism.
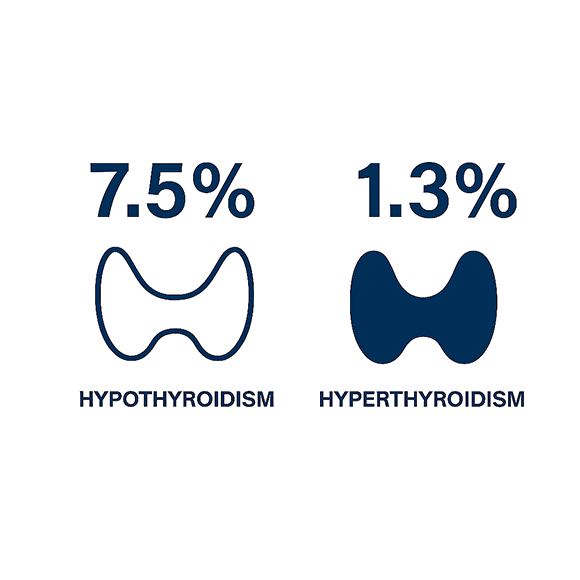
Subclinical Hypothyroidism (SCH) represents an early, often silent stage of thyroid dysfunction where TSH levels are elevated while T3 and T4 remain normal. Despite its subtlety, SCH is clinically important, as it may progress to overt hypothyroidism and has been linked to cardiovascular, metabolic, and reproductive complications.
Conversely, subclinical hyperthyroidism is defined by suppressed TSH levels with normal thyroid hormone concentrations, also carrying potential risks such as heart rhythm disorders and bone loss.
Globally, thyroid disorders are common and frequently underdiagnosed—affecting up to 15% of women and 8% of men—with women disproportionately impacted.
Early detection and a clearer clinical approach to managing subclinical forms are essential to prevent long-term health consequences and improve quality of life.
1. Vanderpump MP. The epidemiology of thyroid disease. Br Med Bull. 2011;99:39-51. doi: 10.1093/bmb/ldr030. PMID: 21893493. (epidemiology of thyroid disease | British Medical Bulletin | Oxford Academic)
This review shows that thyroid disorders affect up to 10% of adults, with subclinical hypothyroidism occurring in up to 8% of women and being several times more common than overt disease, often remaining undiagnosed.
2. Bernadette Biondi, David S. Cooper, The Clinical Significance of Subclinical Thyroid Dysfunction, Endocrine Reviews, Volume 29, Issue 1, 1 February 2008, Pages 76– 31, https://doi.org/10.1210/er.2006-0043 (Clinical Significance of Subclinical Thyroid Dysfunction | Endocrine Reviews | Oxford Academic)
This review shows that subclinical thyroid dysfunction may progress to overt disease at a rate of about 2–5% per year and is associated with up to a threefold increased risk of atrial fibrillation and bone loss.
Dysmetabolism
Dysmetabolism
The current global epidemic of obesity represents a major medical and public health challenge. Beyond its well-known impact on cardiovascular and musculoskeletal health, obesity has led to a dramatic increase in the prevalence of type 2 diabetes, forming the core of what is now recognized as a dysmetabolic condition. This state is characterized by a complex interplay of insulin resistance, low-grade chronic inflammation, and hormonal dysregulation, which together promote metabolic and vascular complications.
When combined with other inflammation-triggering factors—such as sedentary lifestyle, poor diet, and genetic predisposition—obesity contributes to a systemic imbalance that extends far beyond metabolic disease alone. Despite its growing incidence, this dysmetabolic condition remains underestimated and undertreated, calling for greater awareness, early prevention strategies, and integrated therapeutic approaches to mitigate its long-term consequences on global health.
1. Hotamisligil, G. Inflammation and metabolic disorders. Nature 444, 860–867 (2006). https://doi.org/10.1038/nature05485. (Inflammation and metabolic disorders – PubMed)
This review shows that obesity induces a chronic low-grade inflammatory state, with pro-inflammatory cytokines increased up to 2–3 fold, contributing directly to insulin resistance and the development of type 2 diabetes and metabolic complications.
2. Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006 Dec 14;444(7121):840-6. doi: 10.1038/nature05482. PMID: 17167471. (Mechanisms linking obesity to insulin resistance and type 2 diabetes – PubMed)
This review shows that excess adiposity drives insulin resistance and β-cell dysfunction, increasing the risk of type 2 diabetes by up to 3–7 fold, with substantial loss of β-cell function already present at diagnosis.
Osteopenia / osteoporosis
Osteopenia & Osteoporosis
Osteopenia and osteoporosis are progressive conditions characterized by reduced bone mineral density and deterioration of bone microarchitecture, leading to an increased risk of fractures.
Osteopenia represents the early stage of bone loss and is often considered a therapeutic limbo due to the lack of clear guidelines, the variable fracture risk, and the limited or undocumented efficacy of pharmacological treatments.
From an endocrinological perspective, both conditions reflect complex alterations in hormonal regulation—particularly involving estrogen, testosterone, parathyroid hormone, and vitamin D—that critically influence bone remodeling and calcium homeostasis.
Osteoporosis, the more advanced and clinically significant form, places a substantial burden on individuals and healthcare systems. Currently, among people over the age of 55, there are 37 million fragility fractures, equivalent to about 70 fractures every minute.
Overall, osteoporosis affects more than 500 million men and women worldwide, highlighting the global magnitude of this silent yet preventable endocrine-related disease.
1. Compston, Juliet E et al. The Lancet, Volume 393, Issue 10169, 364 – 376 (Osteoporosis – The Lancet)
This review highlights that osteoporosis affects hundreds of millions of people worldwide and accounts for millions of fragility fractures annually, with fracture risk increasing 2–4 fold for each standard deviation decrease in bone mineral density.
2. Raisz LG. Pathogenesis of osteoporosis: concepts, conflicts, and prospects. J Clin Invest. 2005 Dec;115(12):3318-25. doi: 10.1172/JCI27071. PMID: 16322775; PMCID: PMC1297264. (Pathogenesis of osteoporosis: concepts, conflicts, and prospects – PubMed)
This review describes osteoporosis as an age-related endocrine-metabolic disease, showing that bone mass declines by about 0.5–1% per year in older adults due to an imbalance between bone resorption and formation, leading to increased fracture risk.
